How's your pair hangin'?
Testicular cancer is the #1 cancer in younger guys. But good news: it's highly curable when caught early.
Learn how to give your nuts a feel and get to know what's normal for you. So if you notice a change — or that something doesn't feel right — you'll know to act on it.
How to check your pair
Every nut is unique. Get to know yours in three easy steps.

Warm up in a steamy shower. This relaxes and loosens your nuts, getting them ready to be checked.
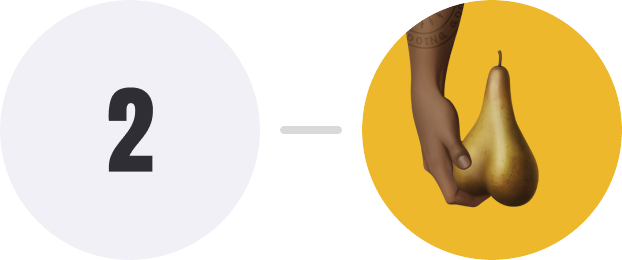
With your thumb and finger, roll one testicle to get to know what’s normal for you. Check for any changes or anything painful.
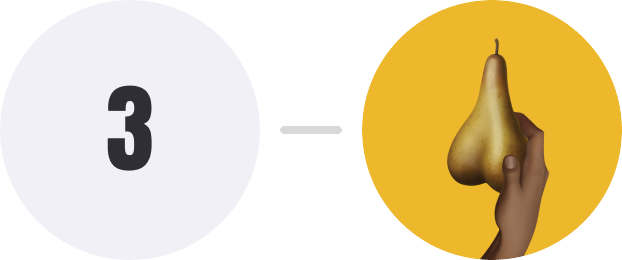
Repeat with the other nut.
What to do next
Get to know what's normal, what's not and when to take action.
What to look for
Your nuts should feel pretty smooth and firm. Sensitive, but not painful. Get to know what’s normal for you. Then look for unusual changes over time. Stuff like a lump, swelling or pain. If you notice a change, it doesn’t automatically mean something is wrong. Get your doc to take a look and go from there.
Found something?
Lumps, bumps and aches can be a normal part of testicle ownership. But if you've noticed something that wasn't there before — or something has changed — it's time to tee up a visit to the doctor. Our guide explains what to expect from your appointment.

Want to know more?

Get the facts about testicular cancer
What is testicular cancer? Who's at risk? Our article answers these questions and – importantly – points you to reliable information.

The tools to tackle testicular cancer
In the unlikely event that you or someone you know is diagnosed with testicular cancer, Movember has your back.
Nuts & Bolts is our go-to website for reliable, straight-talking testicular cancer information, resources and guidance.
Spread the word
See how you can share our Testicular Cancer Awareness Month campaign with your network.